Case Presentation:
A 52-year-old male with metastatic cancer undergoing chemotherapy presented to the Emergency Department with:
● Acute chest pain
● Shortness of breath
Vital signs:
● Respiratory Rate: 26
● O₂ Saturation: 94% (on room air)
● Blood Pressure: 100/65 mmHg
● Heart Rate: 111 bpm
This was the ECG of the patient,
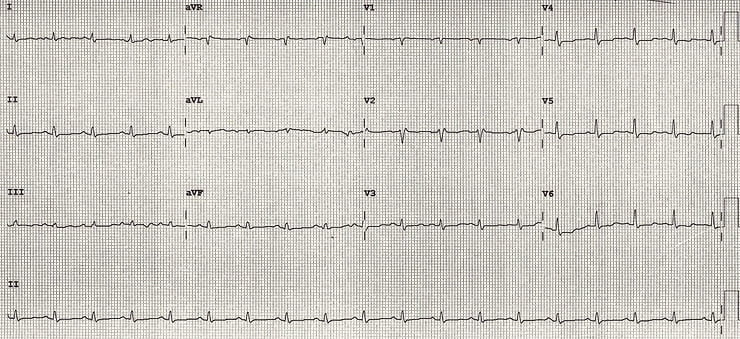
What is your diagnosis?
What is your diagnosis?
Let’s walk through the case as it unfolded in real time.
First Impression: Suspected Pulmonary Embolism
The initial clinical picture strongly suggested PE:
● Active cancer
● Ongoing chemotherapy
● Sudden chest pain + SOB
● Tachypnea and tachycardia
He fit every box for anticoagulation and admission with planned CT Pulmonary Angiogram (CTPA)
But one key detail almost derailed everything…

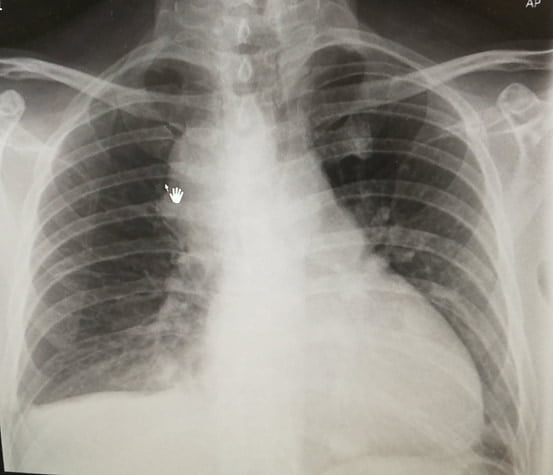
Chest X-Ray Clue
Although the CXR was AP view, cardiomegaly was evident.
This raised concern — and led to a closer look at the ECG.
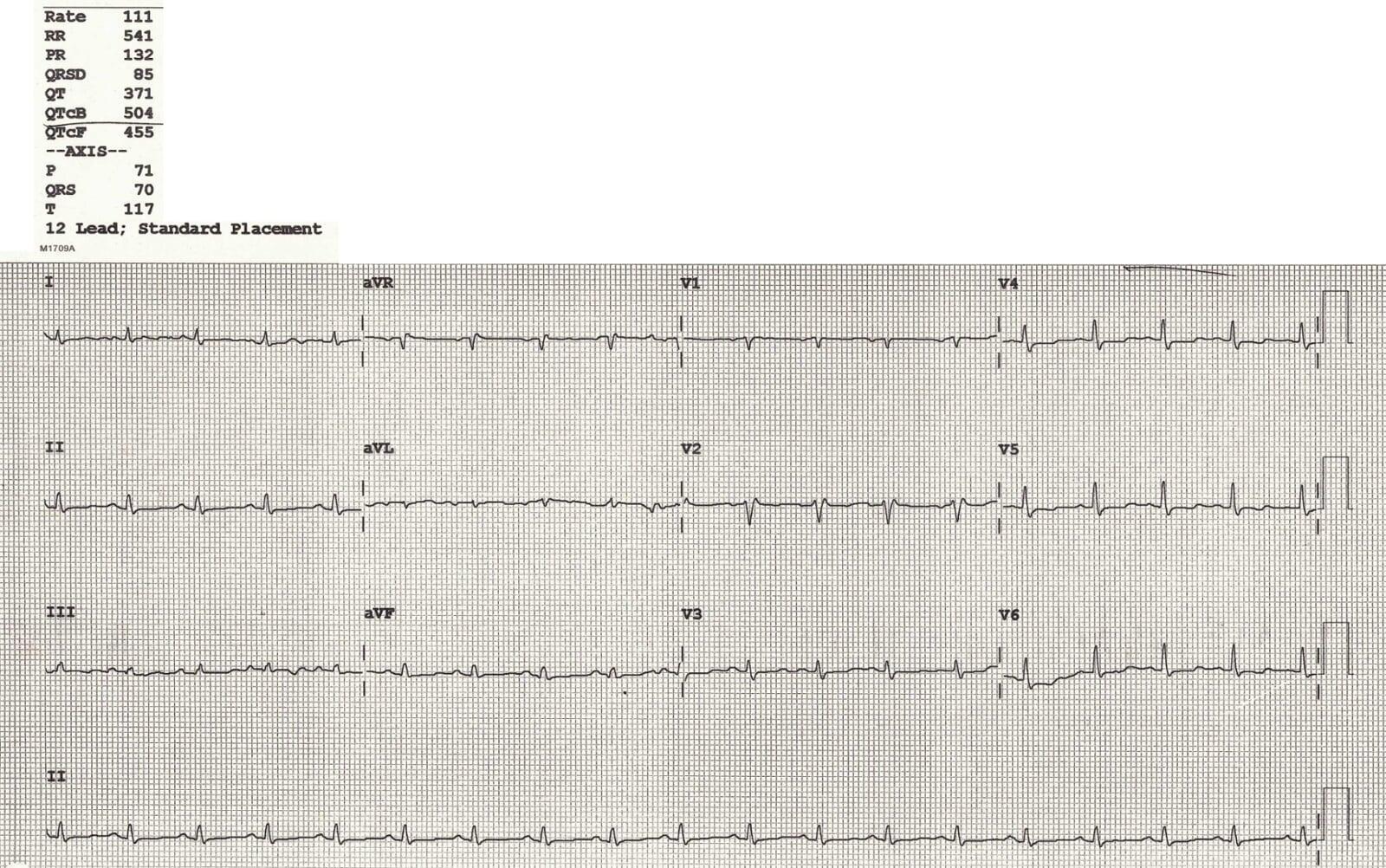
- ECG Findings
- ECG Findings
The ECG showed two critical abnormalities:
- About the Long QT
- Focus: Low Voltage ECG
1. Prolonged QTc
2. Low voltage ECG
● Likely related to chemotherapy
● Electrolytes were not severely abnormal
● Will be covered in detail in another blog
Definition:
● Limb leads (I + II + III) total height < 15 small squares, and/or
● Precordial leads (V1–V3) total height < 30 small squares
Causes fall into two categories:
1) Poor signal generation by the heart:
● Cardiomyopathy
● Hypothyroidism
● Myocardial infiltration (e.g. sarcoidosis)
2) Barriers between the heart and leads:
● Fat (obesity)
● Air (COPD)
● Fluid (pericardial/pleural effusion)
- Pattern Recognition: Tachycardia + Low Voltage
- Pattern Recognition: Tachycardia + Low Voltage
💡 This combination strongly suggests:
Pericardial Effusion
Classic ECG Triad of Massive Pericardial Effusion:
● Low Voltage ECG
● Tachycardia
● Electrical Alternans(not seen in this case)
- Why This Matters?
- Why This Matters?
If this patient had been anticoagulated for presumed PE, he may have deteriorated due to hemorrhagic tamponade from undiagnosed pericardial effusion.
- What Was Done?
- What Was Done?
● Immediate bedside echo was performed → Confirmed pericardial effusion
● CTPA was expedited (to rule out PE before anticoagulating)
● CTPA showed no pulmonary embolism
🟢 Patient was safely admitted to CCU and did well.
- Key Learning Points:
- Key Learning Points:
● Low-voltage ECG is a powerful early clue
● Tachycardia + Low Voltage = Think pericardial effusion
● Don’t treat presumed PE blindly — stop and confirm
● CTPA + Echo combo is crucial when the diagnosis is unclear
Below are the Echo findings of this patient
- 🔗 Further Learning
- 🔗 Further Learning
✅ FAQ – Small, Yet Dangerous
Q1: What are the ECG criteria for diagnosing low voltage?
A1: Limb leads I + II + III < 15 mm combined, or V1–V3 < 30 mm combined.
Q2: What should you consider when dealing with low voltage ECG with tachycardia?
A2: Pericardial effusion is the most serious cause, especially in cancer patients or those with inflammatory conditions.
Q3: Why is anticoagulating blindly in suspected PE dangerous?
A3: In cases like pericardial effusion, anticoagulation may lead to hemorrhagic tamponade and death.