Introduction: The Case Presentation
The Sudden Episode
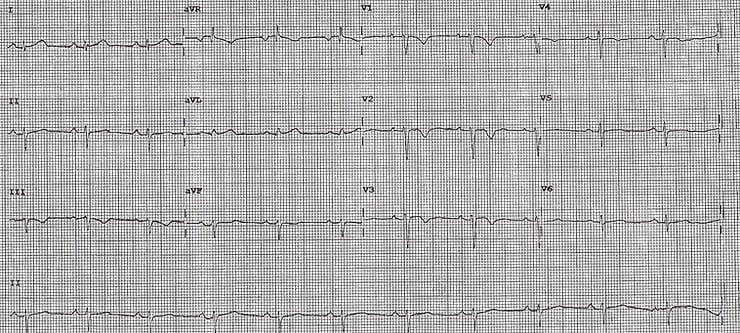
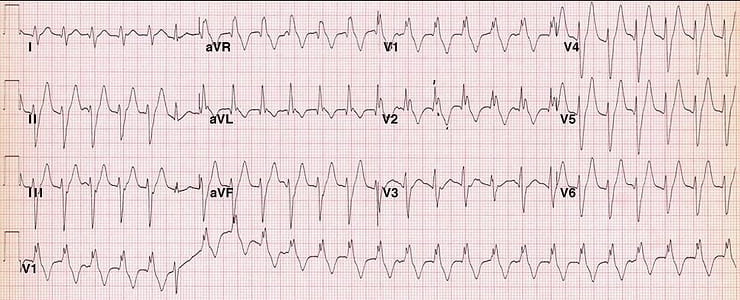
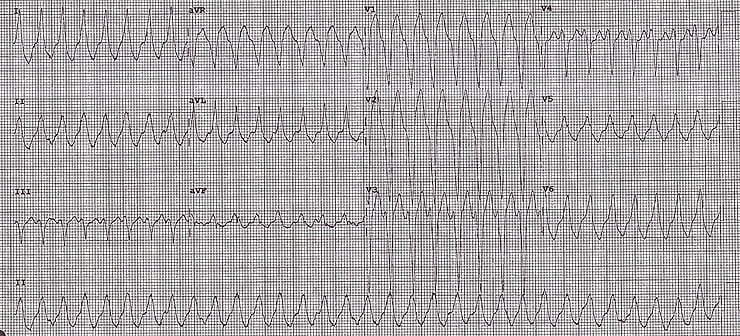
During his visit, the patient suddenly developed another episode of palpitations, prompting the need for a repeat ECG. Here's what was found:
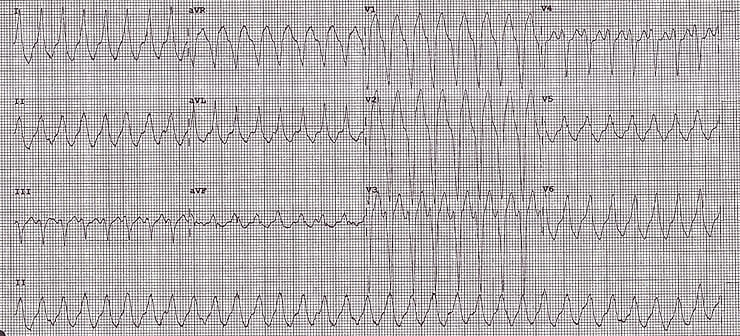
ECG of the patient during the episode
(Courtesy of Dr. Chris Beng, Emergency Medicine Consultant, UK)
Key Diagnosis in Emergency Cardiology: Analyzing Palpitations
This case serves as a great example to discuss differential diagnoses (D.D.) in emergency cardiology, specifically related to syncope, pre-syncope, and palpitations from an ECG perspective.
Differential Diagnoses to Rule Out in Palpitations
Before determining that the ECG is normal, it’s important to rule out:
Acute Coronary Syndrome (ACS)
Arrhythmias and Heart Blocks
Pulmonary Embolism
Abnormal Intervals:
Long/Short PR interval
Long/Short QT interval
Genetic Conditions:
Hypertrophic Cardiomyopathy (HCM)
Brugada Syndrome
Arrhythmogenic Right Ventricular Dysplasia (ARVD)
ECG Analysis
Upon closer examination, the following ECG abnormalities were observed:
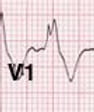
2. Epsilon wave in V2 (a distinctive wave at the end of the complex and beginning of the ST segment)
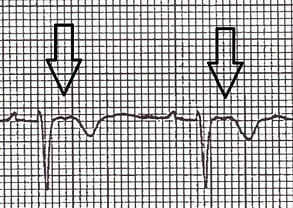
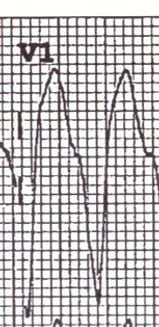
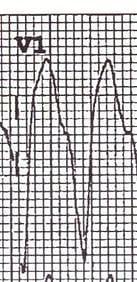
3.L BBB Morphologyin VT ECG (Left Bundle Branch Block)
The Diagnosis: Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
By combining the above findings, the diagnosis of Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC), also known as Arrhythmogenic Right Ventricular Dysplasia (ARVD), was established.
Discussion: Understanding ARVC
Prevalence: ARVC is the second most common cause of sudden cardiac death in young individuals (after HOCM), accounting for up to 20% of sudden cardiac deaths in patients under 35 years of age.
Genetic Information: ARVC is inherited in an autosomal dominant pattern and is more common in men (3:1) and individuals of Italian or Greek descent.
It is estimated to affect 1 in 5,000 people (not as uncommon as one might think).
Pathogenesis of ARVC
ARVC is characterized by fibro-fatty replacement of the right ventricular myocardium, leading to paroxysmal ventricular arrhythmias and sudden cardiac death.
ECG Findings in ARVC
Key ECG findings in ARVC include:
Epsilon wave (30% of patients, most specific finding)
T wave inversion in V1-V3 (seen in 85% of patients)
Prolonged S-wave upstroke in V1-V3 (95% of patients)
QRS widening in V1-V3
Paroxysmal episodes of ventricular tachycardia (VT) with LBBB morphology (right ventricular VT)
Understanding LBBB in VT
In ARVC, when VT occurs, it presents with LBBB morphology. This is due to the right ventricle being stimulated first, leading to the observed pattern.
"VT with LBBB morphology, this means that the right ventricle was stimulated first, which means that the firing focus is in the right ventricle"
"VT with RBBB morphology, this means that the left ventricle was stimulated first, which means that the firing focus is in the left ventricle"
Investigation of ARVC
Echocardiography: Dilated, hypokinetic right ventricle
Cardiovascular MRI: The investigation of choice to detect fibrofatty infiltration and thinning of the RV myocardium.
Treatment Options
Anti-arrhythmic drugs: Beta-blockers (e.g., Sotalol) or Amiodarone
Anticoagulants: To prevent thrombus formation due to right ventricular hypokinesis
Radiofrequency ablation: May be considered for conduction pathway issues
Implantable cardioverter-defibrillator (ICD): For high-risk patients
Cardiac transplantation: In severe cases
ARVC is a good example of a VT that comes from the right ventricle, this is where the pathology is, i.e. (right ventricle is stimulated 1st = same as LBBB = LBBB morphology).
This particular patient was known to have ARVC & all his VTs self self-terminated which made our life much easier.
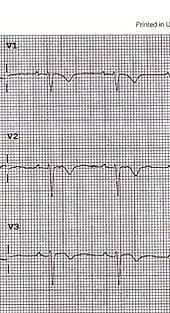
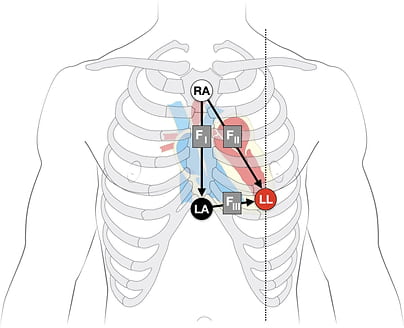
Fontaine leads
Fontaine bipolar precordial leads (F-ECG) are used to increase the sensitivity of epsilon wave detection. Leads are placed as shown:
Right Arm (RA) over the manubrium.
Left Arm (LA) over the xiphoid process.
and Left Leg (LL) in the standard V4 position (5th ICS MCL).
✅ FAQ Section for This Article
Q1: What is Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)?
A1: ARVC is a genetic disorder causing fibro-fatty replacement of the right ventricular myocardium, leading to arrhythmias and risk of sudden cardiac death.
Q2: What are the ECG features of ARVC?
A2: ECG findings include epsilon waves, T-wave inversions in V1-V3, prolonged S-wave upstroke, QRS widening, and episodes of VT with left bundle branch block (LBBB) morphology.
Q3: How is ARVC diagnosed and managed?
A3: Diagnosis involves echocardiography, cardiac MRI, and ECG findings; management includes beta-blockers, antiarrhythmics, ICD implantation, and in severe cases, heart transplantation.
Additional Resources and Video Link
For more information on ARVC, refer to the following resources:
Want to take your ECG skills to the next level?
If this case grabbed your attention, the Emergency Physician’s ECG Course (EPEC) builds on exactly this type of real clinical problem solving, with live teaching, interpretation frameworks, and patterns you’ll use day in, day out in the ED.
Learn how to consistently read tough ECGs with confidence, not guesswork.